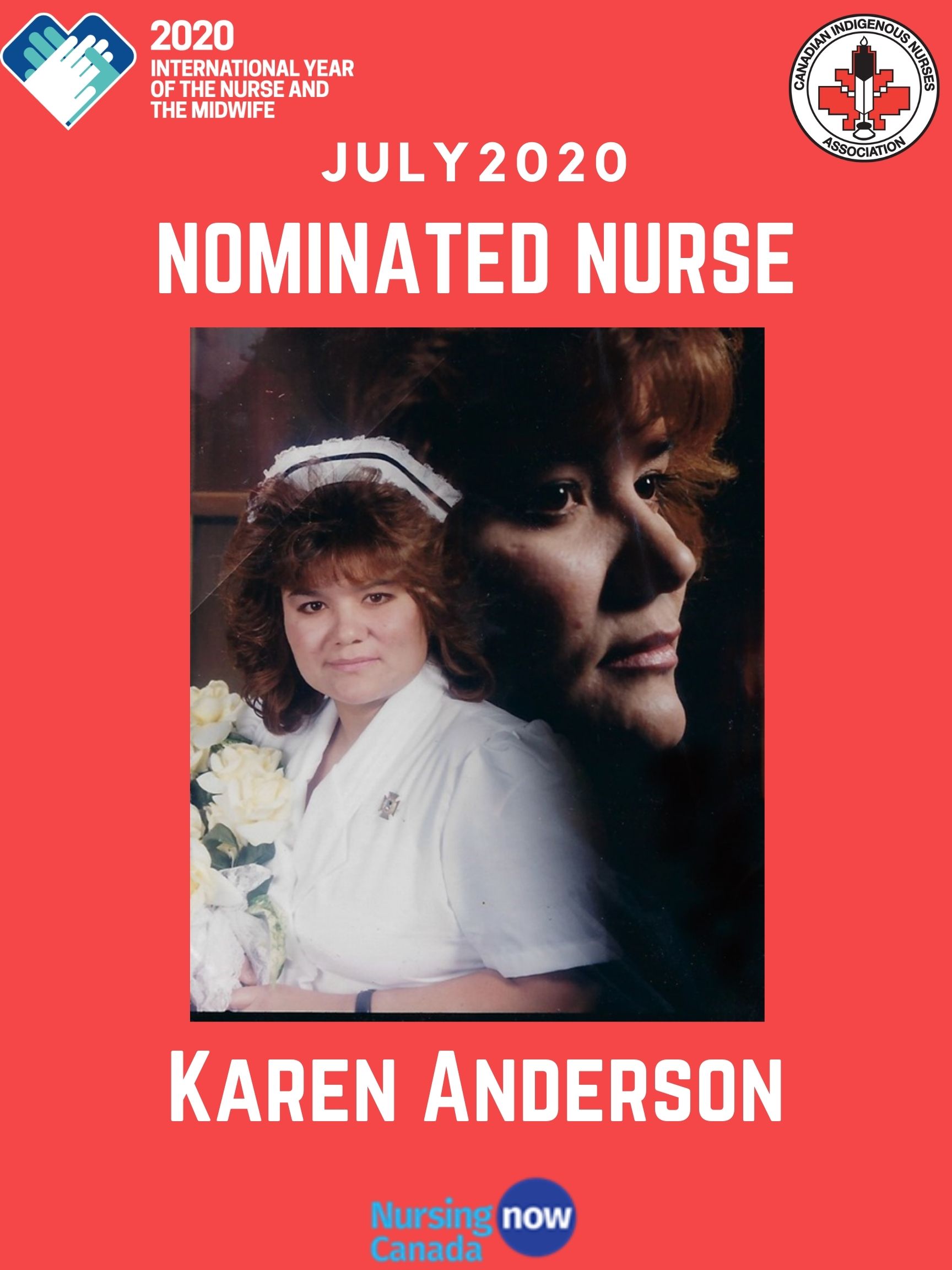
Karen Anderson is the July 2020 featured nurse of the Nominate a Nurse or Midwife campaign!
Karen is a Nurse Practitioner and was nominated by multiple people for her work.
One of Karen's nominators, Amy Thomson, had this to say:
Karen has gone above and beyond the call of duty as a nurse practitioner at OGWADENI:DEO children's aid society. Karen ensures the safety of children by completing comprehensive physical assessments in the families' homes, identifying critical concerns and managing child needs with her services provided. Karen has strived to improve health care to families and children who have come in contact with a child protection agency. This is a new role for nurse practitioners and Karen is leading the way in her profession. Karen has been successful with bringing health services needed to the children she aids in her role at OGWADENI:DEO. During this difficult time of COVID-19, Karen has ensured all staff are provided with correct PPE and current evidence-based research/resources to maintain the safety of clients/families. Karen plays a pivotal rule in the assessment of neonatal babies born with additions, establishes a plan of care for the mother and child to meet the needs of the family. She applies her knowledge of primary care to support and protect children in need through therapeutic communication. Karen has made crucial changes to policies and procedures to advocate for equal rights of children living in foster homes compared to children living with relatives.
In addition, Karen has used her Indigenous experiences and knowledge to develop the Anderson Aboriginal Assessment Model (AAAM). Her theory demonstrates a unique way of approaching traditional knowledge and culturally sensitive care during each assessment interaction with clients and families who have experienced trauma and intergenerational grief. This model when published will be an incredible accomplishment and change the way Indigenous peoples get assessed by the medical community.
Her work cannot go unrecognized and I believe she is worthy of being nominated for the outstanding work she maintains in our community.
A second nominator, Katherine Phillips, said:
I have worked with Karen for close to 20 years. First she was an RN that I worked closely with managing the patients at Jay Silverheels (an inpatient 7 bed ward for patient who couldn't live at home but not appropriate for a nursing home) and home visits. We cared for numerous palliative care patients who chose to die in the community or at Jay Silverheels. I encouraged Karen to apply to NP school as I found her to be an incredibly smart and competent nurse.
Karen went off to NP school where she thrived. When she completed NP school Karen was hired by the family health team that I worked with. Karen worked in this team for 4 years. She was loved by the patients and respected by staff. Karen and I worked very closely together. She would consult with me in order to provide good care to our patients. She played an integral role in care for our native patients.
Karen has also worked extensively in northern reserves, often as the only medical personnel on site. She ran code blues, and dealt with reserves with suicide crisises.
Throughout the years Karen and I have kept in touch often discussing tough and interesting medical cases.
I trust Karen and would gladly have my family see her as patients. I trust her completely.
Karen is now working as a nurse practitioner on Six Nations increasing the healthcare standard for traumatized children. She cares deeply about these children and she wants to make a difference. For example Karen negotiated with a psychologist company so the kids could be seen quickly and begin the healing process. She also negotiated to get a good hourly rate as a bonus.
Karen has also worked to develop a relationship with McMaster Children's Hospital to develop a program for the children to be assessed by paediatric physicians who had experience with maltreatment; the Child-advocacy-assessment program.
CINA recieved a third nomination for Karen from Lindsay Lessard, who said:
Karen Anderson was one of my preceptors during my nurse practitioner program. I was nervous when first meeting Karen (as all students are before meeting their preceptors), however, these feelings were immediately... she was warm and friendly, and she created a safe environment where I did not feel incompetent or dumb. She demonstrated these same characteristics when interacting with all her patients. When caring for patients she took the time to create holistically care plans individualized to each patient’s needs and circumstances. We were working in a community that was of low social economic status, where patients often could not afford a prescription or physiotherapy for example. Karen worked hard to assist her patient’s overcome these barriers by speaking with pharmacists and utilizing appropriate LU codes to allow for more affordable medication. Additionally, she was very knowledgable about resources in the community that offered services such as physiotherapy that were covered under OHIP.
Karen is also great at her job as she ensures her practices are Evidenced based. She engages in several activities such as reviewing guidelines and articles and attending talks and presentations to ensure her practice is up to date.
CINA contacted Karen and asked her about her work as an Indigenous nurse:
Q. How long have you been working in health care? What province/territories do you work in, or have you worked in?
I have been in the nursing field for 27 yrs and for 12 of those years I have been a Nurse Practitioner. I have worked primarily in First Nations communities in BC, Alberta, Manitoba, Ontario and with the Inuit in Nunavut. I currently work in Ontario for OGWADENI:DEO (Indigenous child protection agency) on the Six Nations of the Grand River First Nation. OGWADENI:DEO has recently established a medical team whose focus is to ensure exceptional care for all children in care and to those who come in contact with the agency. OGWADENI:DEO is the first Indigenous child protection agency who saw the need and benefit for a Nurse Practitioner and a Registered Nurse in the agency.
Q. What made you want to become a nurse?
When I was a young woman, I was going to school to learn a trade to become a welder. I was doing my placement in welding through Mohawk College. One day during my placement I was welding overhead not realising that there was a crack in my face shield and had gotten the “welders flash burn.” Both my eyes felt like sand was in them and it was very painful. I had to keep my eyes closed. I went to the hospital. Where a nurse met me at the door and helped me get inside. She must have saw that I was frightened because she stayed with me most of the time I was there. She was very kind and had a calming voice that helped during that stressful time. It was at that moment that I realised I wanted to be a nurse, and so my journey began.
Q. What makes you proud to be an Indigenous nurse?
Being proud to be an Indigenous Nurse Practitioner is rooted in my love for being Indigenous. I come from a great line of Indigenous people and have a responsibility that I have never taken lightly. I am Haudenosaunee, Cayuga Nation, Wolf Clan. My father was a heredity Chief and my great, great grandfather was the last of the heredity Grand Chiefs on my reserve. I attended longhouse with my Grandmother when ever I could. My Grandmother helped many people who needed ceremonies and was very well respected on our Reserve. It was my Grandmother who gave me a love for the People and made me proud to be Indigenous. Her teachings live with me and resonate daily with in me. It has always been an great honor for me to work with my People.
Q. What does it mean to you to be an Indigenous nurse?
As an Indigenous Nurse Practitioner I find that I need to practice in two worlds. I have studied modern medicine/nursing and I also have an understanding of traditional healing practice/ceremonies. I have always identified myself as a person who bring two worlds together.
With my experience and knowledge of Indigenous peoples I was able to develop an assessment model for working with Indigenous People call: Anderson Aboriginal Assessment Model (AAAM). It should be published in mid 2021. AAAM was developed from my years of experiences, knowledge of traditional practices and ways of knowing. The AAAM theory will help none Indigenous peoples to work more effectively, compassionately and increase the standard of care to exceptional care and bring the two worlds together.
On behalf of the team at CINA: thank you Karen for all of your work!
* * *
Do you know of an amazing Indigenous nurse or midwife that you would like to nominate? Check out the campaign page here:

